OUR FERTILTY HOSPITAL
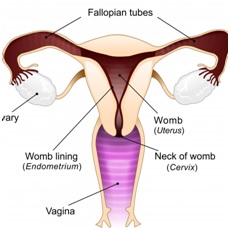
The female sexual organs
The female sexual organs The external organs are known as the vulva. This includes the opening of the vagina, the inner and outer lips (labia) and the clitoris. The woman's internal organs are made up of: The pelvis: this is the bony structure around the hip area, which the baby will pass through when he or she is born. Womb or uterus: the womb is about the size and shape of a small, upside-down pear. It is made of muscle and grows in size as the baby grows within it. Fallopian tubes: these lead from the ovaries to the womb. Eggs are released from the ovaries into the fallopian tubes each month, and this is where fertilisation takes place. Ovaries: there are two ovaries, each about the size of an almond; they produce the eggs, or ova. Cervix: this is the neck of the womb. It is normally almost closed, with just a small opening through which blood passes during the monthly period. Vagina: the vagina is a tube about three inches (8cm) long, which leads from the cervix down to the vulva, where it opens between the legs.
The woman's monthly cycle
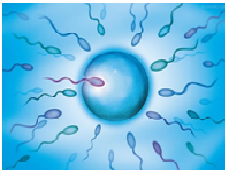
Ovulation occurs each month when an egg is released from one of the ovaries. Occasionally, more than one egg is released, usually within 24 hours of the first egg. At the same time, the lining of the womb begins to thicken and the mucus in the cervix becomes thinner, so that sperm can swim through it more easily. The egg begins to travel slowly down the fallopian tube. If a man and a woman have recently had sex, the egg may be fertilised here by the man's sperm. The lining of the womb is now thick enough for the egg to be implanted in it after it has been fertilised. If the egg is not fertilised, it passes out of the body during the woman's monthly period, along with the lining of the womb, which is also shed. The egg is so small that it cannot be seen. More than 80% of couples where the woman is under 40 will conceive naturally within one year of having regular unprotected sex.
When should u seek gynaecologist help?
If you’ve been trying to conceive for a year or more and you're not pregnant, it’s time to see your gynaecologist.
If you're a woman over 35, – (the decline in fertility speeds up when a woman reaches her mid-30s)
or if you think either of you may have a fertility problem-like irregular periods,or if you've had treatment for cancer or you think you might have had a sexually transmitted infection (STI) see your gynaecologist after six months of trying to conceive.
Your gynaecologist will be able to carry out an initial assessment to check things that may be causing your fertility problems and advise you about what to do next. It's always best for both partners to visit their GP as fertility problems can affect a man or a woman, or sometimes both.
Trying to conceive can be an emotional process, so it's important to support each other as much as possible. Stress is just one factor that can affect fertility.
Questions your doctor may ask
Your gynaecologist will ask you about your medical ,obstetric and sexual history.
Fertility tests for women
If you're a woman, your gynaecologist may:
or if you think either of you may have a fertility problem-like irregular periods,or if you've had treatment for cancer or you think you might have had a sexually transmitted infection (STI) see your gynaecologist after six months of trying to conceive.
Weigh you to see if you have a healthy body mass index (BMI)
Examine your pelvic area to check for infection, lumps or tenderness, which could be a sign of fibroids, ovarian tumours, endometriosis or pelvic inflammatory disease (PID) – see causes of infertility
If you're a man, your gynaecologist may check your:
Testicles to look for any lumps or deformities
Penis to look at its shape and structure, and for any obvious abnormalities
Fertility tests for women

Blood tests
A sample of your blood can be tested for a hormone like thyroid hormone asay, prolactin,DHEAS,Testosterone,sugars etc. If you have irregular periods, you'll be offered a test to measure hormones called gonadotrophins, which stimulate the ovaries to produce eggs.
Ultrasound scan
An ultrasound scan can be used to check your ovaries, womb and fallopian tubes. Certain conditions that can affect the womb, such as endometriosis and fibroids, can prevent pregnancy. Saline sonosalpingography-- A small amount of fluid is injected into your womb through a tube put into the neck of your womb (the cervix). Ultrasound is used to look at the fluid as it passes through the fallopian tubes to check for any blockages or abnormalities If the sonosalpingography suggests a possible blockage, your doctor will refer you to a specialist to discuss further checks, such as a laparoscopy.X-ray
A hysterosalpingogram is an X-ray of your womb and fallopian tubes after a special dye has been injected. It can be used to detect blockages in your fallopian tubes, which may be stopping eggs travelling along the tubes and into your womb.Laparoscopy
Laparoscopy (keyhole surgery) involves making a small cut in your lower tummy so a thin tube with a camera at the end (a laparoscope) can be inserted to examine your womb, fallopian tubes and ovaries. Dye may be injected into your fallopian tubes through your cervix to highlight any blockages in them. This is not done as routine diagnostic test except in patients with high risk for tubal blockage like PID,h/o TUBERCULOSIS IN THE PAST.Fertility tests for men
Tests to find out the cause of infertility in men include:Semen analysis
This is to check for sperm problems, such as a low sperm count or sperm that aren't moving properly or abnormal looking sperms.Chlamydia test
A sample of your urine will be tested to check for chlamydia, as it can affect fertility. Your gynaecologist will prescribe antibiotics if you have Chlamydia.BLOOD TESTS-HIV,HBSAG,ANTI HCV,THYROID FUNCTION,BLOOD SUGAR.
Types of fertility treatment
No single fertility treatment is best for everyone. The right treatment for you will depend on your circumstances, including the cause of your fertility problems, the age of the female partner and your medical history. Broadly speaking, fertility treatments fall into three categories.Fertility medicines
Fertility medicines are usually prescribed to women as they are mostly used to help with ovulation problems. But, in some cases, they may also be prescribed to men.Common fertility medicines include:
• clomifene/letrozole – encourages the monthly release of an egg (ovulation) in women who don't ovulate regularly or who can't ovulate at all
• metformin – particularly beneficial for women with polycystic ovary syndrome (PCOS)
• gonadotrophins – can help stimulate ovulation in women, and may also improve fertility in men
• gonadotrophin-releasing hormone and dopamine agonists – other types of medication prescribed to encourage ovulation
Surgical procedures
These include fallopian tube surgery, which can be helpful if the fallopian tubes, which lead from the ovaries to the uterus (womb), become blocked or scarred, preventing pregnancy, treating PCO by ovarian drilling,hysteroscopic surgeries for adhesiolysis,septal resection ,polypectomy, lap myomectomy,lap endometriosis cytectomy etc.IN MALES for Correcting an epididymal blockage and surgery to retrieve sperm etc.
Assisted conception
This can include intrauterine insemination (IUI), in which sperm is placed into the womb using a fine plastic tube. This can be helpful in cases of mild sperm problems. Intrauterine insemination (IUI) is a fertility treatment that involves directly inserting sperm into a woman's wombFertility tests before IUI
For a woman to have IUI, her fallopian tubes (the tubes connecting the ovaries to the womb) must be open and healthy. You and your partner won't usually be offered IUI if you have:• unexplained infertility
• a low sperm count or poor quality sperm
• mild endometriosis
This is because there is some evidence to suggest that it won't increase your chances of getting pregnant in these circumstances compared with natural attempts.
Timing your IUI treatment
You may be offered IUI in a natural (unstimulated) cycle or in a stimulated cycle.To increase your chances of success, a cycle of IUI should be carried out just after ovulation. Ovulation usually happens between 12 and 16 days after a woman has had their period, if you have a regular menstrual cycle. This can vary if you have an irregular menstrual cycle.
You may be offered Follicular study ultrasound to an predict ovulation.
Stimulated IUI
Sometimes, fertility medicines are used to stimulate ovulation before IUI.In this case, vaginal ultrasound scans are used to track the development of your eggs. As soon as an egg is mature, you'll be given a hormone injection to stimulate its release.
Fertility tests for women
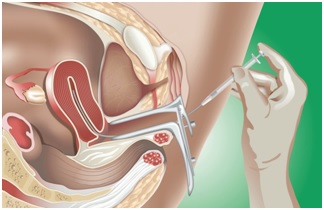
If a couple decides to have IUI using their own sperm, the man will be asked to provide a sperm sample at the fertility clinic by masturbating into a specimen cup. This usually happens on the same day that IUI treatment takes place. The sperm sample will be "washed" and filtered to produce a concentrated sample of healthy sperm. An instrument called a speculum is inserted into the woman's vagina to keep it open. A thin, flexible tube called a catheter is then placed inside the vagina and guided into the womb. The sperm sample is then passed through the catheter and into the womb. This process is mostly painless, although some women experience mild cramping for a short while. The process usually takes no more than 10 minutes. You should be able to go home after a short rest.
IUI using donor sperm
Frozen sperm from a donor can also be used for IUI.
Your chances of success with IUI
This depends on lots of different things, including:
the cause of infertility
the woman's age
the man's sperm count and sperm quality (using fresh sperm leads to higher conception rates than using frozen sperm)
whether or not fertility medicines are used to stimulate ovulation (this can increase your chances of success). There are many different factors involved, so it's best to talk to your fertility team about your individual chances of success.
Are there any risks?
Some women have mild cramps similar to period pains, but otherwise the risks involved with IUI are minimal. If you take a fertility medicine to stimulate ovulation, there is a small risk of developing a condition called ovarian hyperstimulation syndrome. There's also a chance that you will have more than one baby, which carries additional risks for both you and your babies Assisted conception also includes IVF (in vitro fertilisation), in which sperm and eggs are mixed outside the body and put back into the womb. This can be helpful for a range of fertility problems, including more severe sperm problems and cases of unexplained infertility. In vitro fertilisation (IVF) is one of several techniques available to help people with fertility problems have a baby.
It can be carried out using your eggs and your partner's sperm, or eggs and/or sperm from donors.
Who can have IVF?
Male factor Infertility – Oligozoospermia, Teratozoospermia , Athenozoospermia
Unexplained infertility – When no cause is found.
Tubal blockage – Tuberculosis, Pelvic inflammatory diseases.
Premature ovarian failure – Stopped menstruating / Post-menopausal
Donor cycles – Donor eggs, Donor embryos, Frozen transfers
Surrogacy services – complete till delivery
What are the risks?
There are also a number of health risks involved, including:
side effects from the medications used during treatment, such as hot flushes and headaches
multiple births (such as twins or triplets) –
an ectopic pregnancy – where the embryo implants in the fallopian tubes, rather than in the womb
ovarian hyperstimulation syndrome (OHSS) – where too many eggs develop in the ovaries
What happens during IVF
For women
Step one: Preparation for IVF
Preparation for IVF includes testing for hormones like FSH, LH, Estradiol, AMH, TSH, Prolactin. Hysteroscopy will be recommended to test the uterine cavity before performing IVF. Semen analysis will be done and if any pus cells or signs of infection is present, then we may give the husband an antibiotic. Semen freezing may be required as a backup for IVF.
This helps us when the husband is unable to give sample in case of stress or difficulties on the day of egg retrieval.

Step two: boosting the egg supply
Controlled ovarian stimulation using fertility hormone called follicle stimulating hormone (FSH)/HMG. This is another daily injection you will be given , usually for about 10-12 days.
FSH increases the number of eggs your ovaries produce. This means more eggs can be collected and fertilised. With more fertilised eggs, the clinic has a greater choice of embryos to use in your treatment.
Step three: checking progress
The clinic will keep an eye on you throughout the treatment. You will have vaginal ultrasound scans to monitor your ovaries. We may ask you to provide hormone tests if needed to assess the response. On 5th or 6th day one more injection called an Antagonist (Cetrorelix) may be started to prevent premature follicular rupture. Based on the ultrasound follicular growth report, hormone injections will be adjusted.
About 34-38 hours before your eggs are due to be collected, you'll have a final hormone injection that helps your eggs to mature.

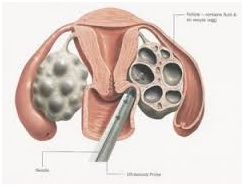
Step four: collecting the eggs
You'll be sedated and your eggs will be collected using a needle that's passed through the vagina and into each ovary under ultrasound guidance. This is a minor procedure that takes about 15 to 20 minutes.
Some women experience cramps or a small amount of vaginal bleeding after this procedure.
Step five: fertilising the eggs
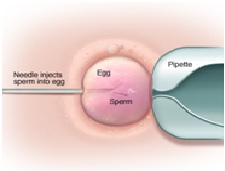
Fertilization process can be carried out by using IVF / ICSI .
IVF-The collected eggs are mixed with your partner's or the donor's sperm in a laboratory. After 16-20 hours, they're checked to see if any have been fertilised.
Step five: fertilising the eggs
ICSI-intracytoplasmic sperm injection-. In case of ICSI, individual selected sperms will be injected into the egg. On day 2/3 embryos will be checked and planned for embryo transfer. If Day 5 transfer is required further culture will be performed for 2/3 more days.
The best one or two embryos will be chosen for transfer. After egg collection, you will be given hormone medicines to help prepare the lining of the womb to receive the embryo. This is usually given either as a pessary (which is placed inside the vagina), an injection, or a gel. After egg collection, you will be given hormone medicines to help prepare the lining of the womb to receive the embryo. This is usually given either as a pessary (which is placed inside the vagina), an injection, or a gel.
Step six: Embryo Transfer
A few days after the eggs are collected, the embryos are transferred into the womb. This is done using a thin tube called a catheter that's passed into the vagina. This procedure is simpler than egg collection and similar to having a cervical screening test, so you won't normally need to be sedated. The number of embryos that will be transferred should be discussed before treatment starts. It usually depends on your age. If any suitable embryos are left over, they may be frozen for future embryo transfers.
For men
Around the time your partner's eggs are collected, you'll be asked to produce a fresh sperm sample. The sperm are washed and spun at a high speed, so the healthiest and most active sperm can be selected. If you're using donated sperm, it's thawed before being prepared in the same way.
Finding out if you're pregnant
Once the embryos have been transferred into the womb, you'll be advised to wait around two weeks before having a pregnancy test, to see if the treatment has worked.If you do become pregnant, ultrasound scans will be carried out during the following weeks to check things are progressing as expected. You will then be offered the normal antenatal care given to all pregnant women.
High tech lab equipment are used in the in vitro fertilization process.
Our FERTILTY TREATMENT success rate is unmatched. We have been getting consistently good pregnancy rate every month as its tailormade , individualized and personalized approach.
Why are our success rate- the best ?
In-house embryologist
- Daily working lab
- Individual attention
- Freezing of super-numerary embryos to increase success
- Laser hatching of embryos if the zona is thick to improve the hatching rate
- Blastocyst culture and transfer
